
Medical Waste Incineration and Dioxin Emission
Proper management of medical waste is fundamental to safeguarding both public health and the environment. While incineration has been employed for decades as a primary method of disposal worldwide, it also carries serious risks. When not properly designed or operated, medical waste incineration is a main source to generate invisible but extremely dangerous byproducts — most notably dioxins and furans, among the most toxic compounds known.
What is Dioxin
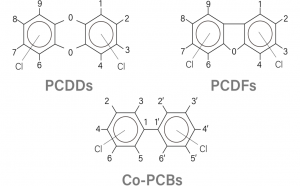
“Dioxins” are a group of chemically related compounds:
- Polychlorinated dibenzo-p-dioxins (PCDDs) and
- Polychlorinated dibenzofurans (PCDFs).
classified as persistent organic pollutants (POPs) that unintentionally produced during the incineration of waste containing chlorine
(e.g. PVC plastics). They are colorless, odorless, and highly toxic even at trace levels.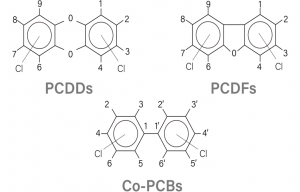
- Highly toxic:Known to cause cancer, reproductive and developmental problems, and damage to the immune system
- Persistent:Remain in the environment for years.
- Bioaccumulative:Build up in the food chain, especially in animal fats.
Even small amounts of dioxin exposure can have significant health impacts. The World Health Organization has listed dioxins among the most dangerous environmental contaminants.
How is Dioxin Formed
Dioxins are unintended byproducts formed during combustion processes involving chlorine, oxygen at a temperature range. The formation in medical waste incinerators is a complex chemical process, but it can be broken down into three key requirements:
- The Necessary Requirements
For dioxins to form, three basic elements must be present:
- Chlorine:from PVC, chlorinated disinfectants, saline residues, etc. No chlorine, essentially no dioxin formation.
- Oxygen:Readily available from the air used for combustion.
- Temperature window:dioxins are dramatically formed within the temperature range 300-500C. In the hot furnace (typically above 850°C, chlorine and carbon compounds break apart. However, during cool down, they pass through this critical temperature range. This is where the most significant dioxin formation occurs.
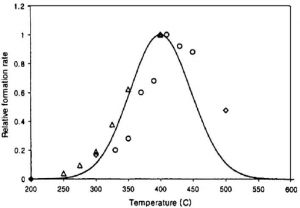
Source: Relative formation rates of dioxins (relative to 400°C case) at different flue gas temperature (McKay, 2001).
Why Medical Waste Incineration Generates Dioxin?
Medical waste often meets an abundance of all these requirements to generate dioxin:
- a significant proportion of plastics, disinfectants, and chemical residues.
- Oxygen presence.
- In incinerators that do not reach and maintain the necessary high temperatures (850–1100 °C) or lack adequate flue-gas cleaning systems, combustion is incomplete. This creates a perfect scenario for dioxin generation.
Once emitted, dioxins disperse into the air, settle on soil and vegetation, and eventually enter the food chain. Unlike many pollutants, they do not degrade easily, making even small releases a long-term environmental and public health concern.
Different types of incineration used
- Open Burning
- Conducted in pits or rudimentary chambers without emission control.
- Burning uncomplete and in limited temperature, producinglarge amounts of smoke, toxic particles, and extremely high levels of dioxins.
- Still practiced in under-resourced regions, but considered the most hazardous and outdated method.
- Small Incinerators
- Used by small hospitals or rural clinics.
- Often operate at insufficient and unstable temperatures.
- Limited or no gas treatment systems.
- Appear controlled but can be dangerous sources of dioxin emissions if not engineered to international standards.
- Large-Scale Incinerators
– Rotary kiln, gasifier (called pyrolysis incinerators sometime)
- Properly designed Industrial facilities with advanced and complex flue-gas treatment processing high volumes of medical waste can reduce risks significantly.
- The necessarity to have strict operational control and facilities are well maintained by a professional operation team.
- High operation and maintenance cost to meet international emission standards.
- Even though, large-scale systems emit harmful levels of pollutants and leave toxic ash.
Dioxin Emission from Medical Waste Incineration
WHO / UNEP Guidelines on Best Available Techniques and Best Environmental Practices (2006) → recommend the same 0.1 ng TEQ/Nm³ limit for medical and hazardous waste incineration.
| Technology | Typical Operating Features | Reported Dioxin Emission (ng TEQ/Nm³)* | Compliance with International Standard (≤0.1 ng TEQ/Nm³*) |
| Open Burning (Direct Combustion) | Waste burned in open pits or rudimentary chambers, no control, without after burner | Over 4,000 | ❌ Exceeds standard by thousands of times |
| Small-Scale Incinerators | Utilizing sufficient temperatures, afterburners and other features | 10 – 500 | ❌ Can be 5,000 thousands of times above limit. Depending on proper operation and maintenance |
| Large-Scale Incinerators (with pollution controls) | Two-stage combustion at >850–1,100 °C, flue-gas treatment | 0.1 – 1.0 | ⚠️ Sometimes compliant, often above |
| State-of-the-Art Incinerators (Best Available Technology, BAT) | High-temp combustion + rapid quench + multi-stage flue-gas cleaning (bag filters, activated carbon, scrubbers) | ≤0.1 | ✔ below 0.1 ng TEQ/Nm³ Significantly high operation and maintenance cost |
Source: Findings on an Assessment of Small-scale Incinerators for Health-care Waste – WHO
The Alternative: Non-Incineration Treatment Technologies
Given the severe health and environmental risks associated with incineration, many countries have shifted toward cleaner, more sustainable methods of managing medical waste. These technologies neutralize pathogens without generating dioxins or other hazardous air pollutants, making them safer both for communities and the environment.
Autoclaving (Steam Sterilization)
- Usinghigh-temperature, pressurized steam to sterilize medical waste, effectively eliminate all microorganisms, including resistant pathogens.
- Generates no dioxins or furans, making it a much safer alternative.
- Produces negligible emissions and is highly cost-efficient compared toState-of-the-Art incineration technologies.
- The safest proven sterilization method over decades in human history.
The U.S. Case: From 6,000 Incinerators to Autoclaves
In the 1990s, the United States operated approximately 6,000 medical waste incinerators. However, the implementation of the Clean Air Act Amendments of 1990 and the subsequent 1997 EPA regulations on hospital/medical/infectious waste incinerators (HMIWIs) drastically changed this landscape. Once stringent dioxin emission limits and monitoring requirements were enforced, many incinerators were shut down or replaced with safer treatment methods. After years of technology evaluation, high-vacuum autoclaving emerged as the dominant solution. Today, over 90% of medical waste in the U.S. is treated by autoclaving.
Other Non-Burn Alternatives
Microwave disinfection: Uses microwave energy to heat and disinfect waste. The production cost is relatively low, and it is mostly used in small equipment with low disinfection requirements, and is rarely used in centralized treatment plants or big capacity projects.
Chemical disinfection: Employs chemical agents (e.g., chlorine compounds) to inactivate pathogens. The cost is very low, but due to the problem of secondary pollution, it is rarely used now..
Thermal treatment (non-incineration): High-temperature methods such as friction heat, very limited application with low capacity and low disinfection requirements.
A Safer Way Forward
At Gient, we are committed to providing safe, environmentally responsible medical waste treatment solutions that eliminate the dangers of dioxins and other toxic emissions.
